Leveraging Non-Denial, Collaborative Programs to Improve Outcomes
HealthHelp, a WNS Company, is a leader in specialty benefits management, has produced a new white paper in conjunction with Xtelligent Health Media, detailing the benefits of a non-denial program based on a collaborative educational model that can help health plans and providers deliver the right care at the right time at the right place -satisfying member demands for timely care and ensuring members always get the highest quality care.
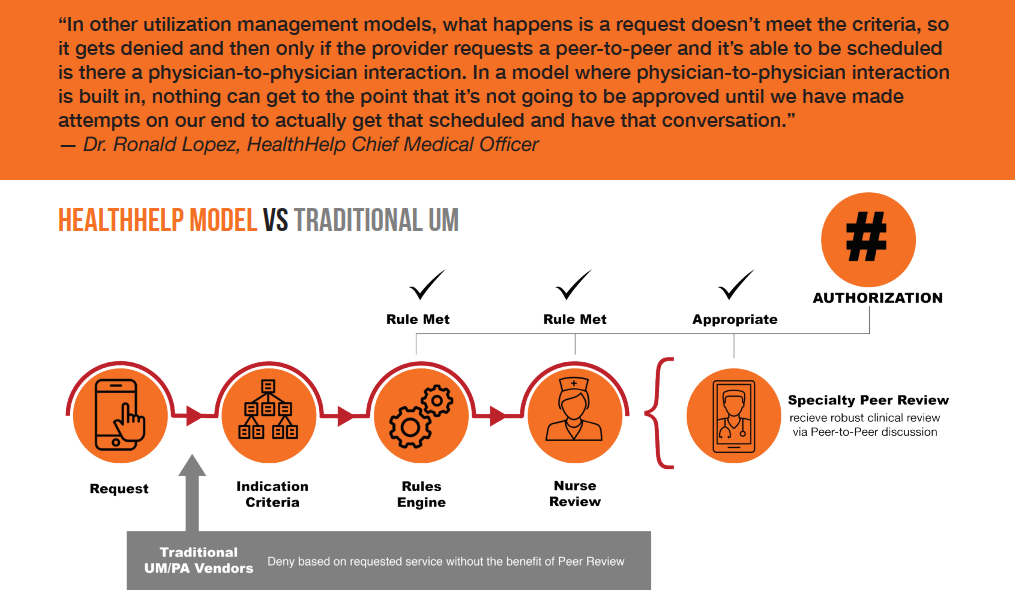
Achieving cost savings by employing traditional utilization management strategies can prove to be a double edged sword for payers. Traditional UM companies lead by denial, potentially creating an adversarial relationship with providers, a situation that can have a negative, trickle-down impact on member satisfaction with their health plan.
Lower Provider Abrasion; Higher Member Satisfaction
There is an alternative method to leverage prior authorization as both a cost savings tool and a means to promote better member outcomes. Download HealthHelp’s new whitepaper, Redefining Utilization Management & Prior Authorization: Leveraging Non-Denial, Collaborative Programs to Improve Outcomes, to learn more.
Highlights include:
- A next-generation approach to utilization management using a “nondenial” program to ensure appropriate and high quality care
- Transforming utilization management from a denial tool to a collaborative educational model that leverages peer-to-peer reviews early and often